The New Gene-Editing Technique That Reveals Cancer’s Weaknesses
CRISPR can finally tell us which human genes are essential—and which matter specifically to cancer cells.
Humans have between 20,000 and 25,000 genes, but which of these really matter? Which are essential, and which are merely optional add-ons?
It’s crazy to me that we still don't know, even though it’s been almost 15 years since the first draft of the human genome was published. Partly, the problem is a technological one. The best way of working out if a gene is essential is to disable it and see what happens, and “we just didn’t have a good way of systematically manipulating genes in humans cells,” says Jason Moffat from the University of Toronto. Sure, scientists have been able to tinker with individual genes, but working through them all, and knocking them out one by one, has been nigh-on impossible.
A technique called RNA interference has come closest. When genes are activated, the instructions encoded within their DNA must first be transcribed into a related molecule called RNA. By interfering with these transcripts, scientists can stop those instructions from ever being realized. But this technique is imperfect: It often fails to silence genes entirely, and it sometimes silences the wrong gene. “That technology allowed us to uncover some of the essential genes but our confidence wasn’t super-high,” says Moffat.
Enter the revolutionary gene-editing technique called CRISPR, which was invented billions of years ago by bacteria, as part of a defense system for hacking into the genes of invading viruses. But in the last five years, scientists have repurposed it into a tool that can edit any gene at will. Unlike RNA interference, which disables the messages transcribed from genes, CRISPR alters the gene itself. It’s like changing the actual text of the book, rather than just gagging someone who’s reading from it. And these changes are very specific—CRISPR rarely misses its target.
Two different groups, one led by Moffat and the other by David Sabatini at the Whitehead Institute for Biomedical Research, have used CRISPR to systematically inactivate almost every gene in human cells in a bid to identify all the essential ones.
Though their studies differ slightly in their details and results, they both illustrate the true power of CRISPR. Amid much hand-wringing about far-flung and grandiose applications, like creating designer babies or engineering malaria-fighting mosquitoes, scientists are already using this technique to revolutionize our basic understanding of the living world. In a single experiment, researchers can quickly do what their predecessors took years to accomplish.
“This is now the most powerful system we have in biology,” says Sabatini. “Any biological process we care about now, we can get the comprehensive set of genes that underlie that process. That was not possible before. There was no way one could imagine doing that.”
CRISPR involves two components—an enzyme called Cas9 that slices DNA, and a guide molecule that deploys Cas9 to the right target. Moffat and Sabatini’s teams both created libraries of guides, targeted to the majority of human genes. Both used the libraries to unleash Cas9 upon individual genes, to see if their loss would affect a cell’s ability to grow or reproduce. And both computed a kind of essentiality score to measure how critical the various genes are.
The two teams identified between 1,600 and 1,800 genes as being essential—around one in ten of the ones they analyzed. “It's a big treasure chest of results,” says Moffat.
Compared to their more dispensable peers, these genes are more strongly activated, and unlikely to carry disabling mutations. They’re more likely to have similar (and equally indispensable) counterparts in other species. And as Moffat puts it: “Essential genes like to hang out with each other.” That is, they build proteins that unite to form large collaborative complexes.
Predictably, the essential genes tend to be involved in fundamental biological processes, like copying DNA, transcribing genes, and building proteins. Perhaps less predictably, Sabatini found that we have no idea what 18 percent of the essential genes on his list are doing—a testament to how much we still have to learn about the most critical parts of ourselves.
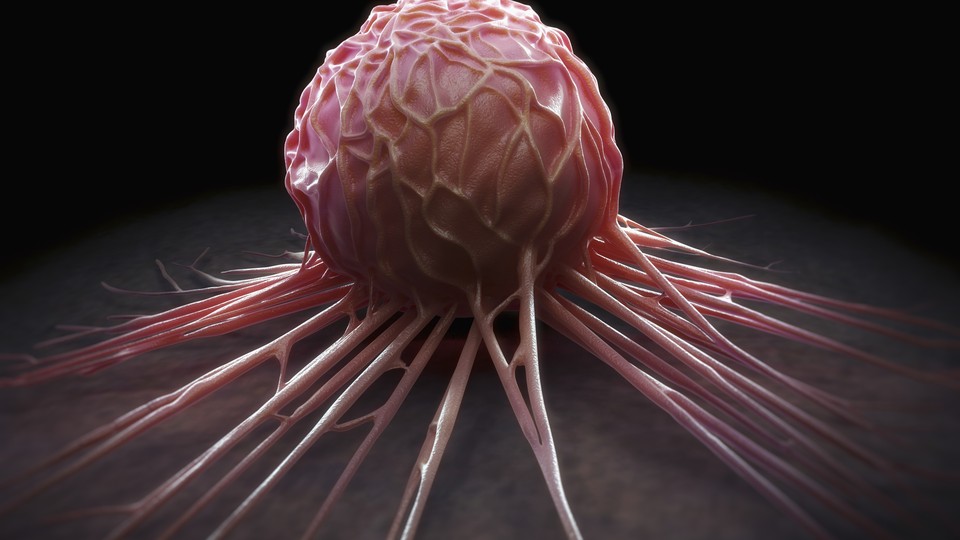
The two teams are also trying to discover genes that are essential in specific contexts. Moffat likens this to a daisy: The core represents genes that are always necessary, while the petals represent those that are important, say, when cells are growing or reproducing, or in one type of cell but not another. CRISPR makes it easy to analyze both the core and the petals. “Anything we can detect in a dish, like whether a cell is square or red, we can find the genes that underlie that,” says Sabatini. “And if you're interested in cancer, you can say: Give me the genes that each type of cancer, and only that type of cancer, cares about.”
Cancer is foremost on his mind. His team has already catalogued the essential genes in four cancer-cell lines, taken from patients with leukemia and lymphoma. Meanwhile, Moffat analyzed cell lines grown from cancers of the brain, colon, skin, and cervix.
Their goal was to find genes that are expendable in healthy cells but crucial in specific types of tumors. These genes represent the box of tricks that cancers use to thrive in the body. They also represent weaknesses that scientists can exploit to destroy cancer cells without harming normal ones. For example, Moffat predicted that some of the colon-cancer cells he studied would be vulnerable to a drug called metformin, while another group would succumb to linezolid—and he was right on both counts.
“We’ve known for many years that the molecular drivers of tumors vary from cancer to cancer and even patient to patient, but we have previously lacked the tools to tackle these differences in a systematic way,” says Feng Zhang from MIT, one of the pioneers of CRISPR. “[These groups] show that CRISPR-based tools are up to the job.”
“My only fear is that we won't find a huge number of genes that differentiate cancer cells and non-cancer cells, and the ones we find won't be druggable,” says Sabatini. “But we need the answer. And if those genes are there, we can find them. It'll just take industrializing this approach, with not just tens of cell lines but hundreds.”
Such work is already underway. Scientists at the Broad Institute and the Dana-Farber Cancer Institute have launched Project Achilles—an initiative that will use CRISPR to search for specific weaknesses in over 500 cancer-cell lines.
“This is a great demonstration of the impact of CRIPSR,” says Aviv Regev at the Broad Institute. “It’s truly better than the tools we had before; it lets us ask crisp questions and get precise answers.” It’s also increasingly versatile, she says. Although scientists initially used it to delete genes, they can now use it to switch genes on, or to gently turn their activity down a notch.
But even CRISPR has its limits. Sabatini says that it’s not great for studying regions of the genome that have been copied many times over. According to few upcoming papers, when CRISPR targets these amplified regions, it cuts all the copies and induces a generic toxic response in the affected cell. “Almost all human cancer lines have amplifications,” says Sabatini, “so if you want to know what the genes there are doing, you can't do it through CRISPR.” Or, at least, not yet.