Since almost the beginning of the pandemic last winter, Harvard’s Michael Mina has been among the country’s most outspoken epidemiologists, urging the public-health Establishment toward a more responsive and creative approach to managing the pandemic, particularly focused on deploying rapid COVID tests, similar to home-pregnancy tests, to help curb the virus’s spread. In October, I spoke to him about the very scary seasonality of the disease and the country’s complacency about it. In December, we talked about the maddening continuing resistance among the medical Establishment to rapid tests, as well as the risks of counting on the efficacy of vaccines, given how little time we’d observed them. We spoke again this week, with a new administration promising a rollout of more rapid testing and vaccine distribution in full swing, but the threat of new strains on the horizon.
How do you see the state of things, right now? I’m having a hard time sort of juggling the bad news about strains versus the good news about vaccines and the trajectories going down. How about you?
Well, my personal feeling is we are seeing the benefits of seasonality hit, which I know some of my colleagues don’t necessarily agree with. But it’s not uncommon for coronaviruses to essentially start dropping around now. Most of the known coronaviruses have something on the order of a three-month window where they’re really infectious — when they’re really transmitting.
And that’s more or less what we were expecting would happen, or at least what I was expecting would happen, in the fall. In the summer, when a lot of people were saying, “This might not be a seasonal virus,” it was just so obvious to me that this was going to hit harder in the fall and that we needed to prepare for that. Now, I think the corollary is that there’s no reason to think that infection rates wouldn’t drop a few months later, just like all of the other coronaviruses. We don’t fully appreciate or understand why seasonality works like this, but if the trajectory stays this way and we also start to achieve some level of herd effects or herd immunity, I think the next few months could start to offer a reprieve. Ideally that will last through the summer until we get into next fall, when we’ll probably have another wave of it. The wild card, of course, being the variants.
You didn’t mention the vaccines. How significant do you think they will be in terms of changing the course of the disease?
Well, I think the most important thing is we’re going to get a lot of the elderly people and vulnerable people vaccinated. But I’ve been very, very disappointed at how the vaccine rollout has gone thus far.
Because of the slowness?
Because of the extremely medical-centric view of prioritizing doctors and health staff above everyone else — especially considering the mantra for so long has been that doctors don’t even need to get tested regularly, PPE is working, don’t worry about it. Then the moment the vaccine comes out, it’s like doctors are at extremely high risk and need to get vaccinated immediately. We spent weeks vaccinating health-care workers we could’ve spent vaccinating the most vulnerable. In the hospitals, they were vaccinating 20-year-olds who are sitting behind a computer and don’t even see patients. And there are patients in the same hospitals who are 65 years old at very high risk of getting COVID who have to wait.
What about now that we’ve mostly gotten through vaccination health workers?
Vaccines are now starting to get to the more vulnerable populations, and I believe that that’s going to start quickly changing the risk-benefit ratio. I don’t think it’s going to change the type of testing we’re going to need to be doing all the time. But I do think we’ll see hospitalizations drop. From there, we need to have a hard discussion about, “Okay, now that we have the vulnerable people vaccinated, what is our endgame here?”
What is the endgame, do you think?
I still to this day have not heard a goal for testing and for vaccination. More broadly, are we trying to get COVID to zero or are we trying to get COVID to a point where it’s palatable for society, it’s not overburdening the hospitals, and it’s essentially looking like flu? Those are really different things. If it’s to get it to zero, we’re in for a really long haul.
It seems to me that getting to zero seems, you know, more or less impossible. We don’t really know exactly what the herd-immunity threshold is, but given some of the higher numbers that have been quoted, given vaccine hesitancy, given the fact that even the vaccines we have are reducing transmission but not eliminating it, it would be very hard to get all the way to zero.
Yeah. And I don’t think zero is what we should be aiming for. It’s really easy to just continue being afraid, but at some point we need to take a step back and say, “Okay, where are we now, and where are we going?” If the goal is just to stop the vast majority of hospitalizations, that might not take very long. At that point, do we keep society shut down just to stop a small number of hospitalizations and deaths?
When you say that if our goal is to reduce the mass majority of hospitalizations that we might hit that goal relatively soon, what do you mean by relatively soon?
Certainly over the coming couple of months, we’re going to see a massive number of the most vulnerable people who make up the majority of deaths become vaccinated. Then all of a sudden mortality and the real damage done by this virus go way down at the aggregate level. People will still talk about long-haulers, long COVID and children getting severe disease. But we have to recognize that, especially in younger people, these are fairly rare events, especially in kids.
And then it’s time to really reevaluate. I do think we should take the summer and do what we didn’t do last year, which was squander the summer and did nothing to prepare for the fall. I think we could take this summer and we could say, “Okay, let’s get all the pieces in place. Let’s get rapid testing ready and rolled out so that society is comfortable with it.” It doesn’t mean people have to rapid test all the time, but if you start to see an outbreak occur, then you get a text message that says, “Hey, start rapid testing again.” We can really set ourselves up as a country to be adaptive, to be able to combat an outbreak when it starts, so that we’re not always playing catch-up after it does. That could allow us to both simultaneously get back to work and get back to school with minimal risk.
On the one hand, it’s pretty easy to imagine that level of normalizing, looking just at the American context. But given that the rest of the world is awaiting vaccinations, and will be waiting in some countries probably for several more years, we’d still be at risk of new strains arriving in the country, right? To me that is an even stronger argument for rapid testing, which could be used as a screening method in lieu of closing borders periodically.
I wanted to ask about the vaccines, though. When we last talked, you were worried that we had evaluated vaccine efficacy so quickly we might be overestimating how powerful the vaccines were — the immune response might wane after a few more months, you said. Are there other problems you’re seeing with our evaluation of the vaccines?
The entire evaluation process was based on symptomatic disease. The major trials didn’t even consider transmission. They didn’t even consider, do we need two doses or one, and what would it mean if we actually could get by for six months between doses, what would that mean for the globe? Does that mean we could actually vaccinate an extra billion people in a year? Well, that’s a massive, massive win for public health if we could, but we didn’t even include it in the trial. We just followed the regular playbook we’ve always used, which is to do a phase three trial, accelerated a little bit. But then the readout was purely, of people who get two doses, what was their ability to not get sick? Why did we not swab people’s noses during those trials, to allow us to ask the basic question, will these vaccines inhibit transmission? That would have massive implications for who we vaccinate first. And we still don’t know the answer.
Another issue: All of the major vaccines that we are building all present the exact same spike protein. They’re all clones of each other — no difference for the most part. Nobody ever took a step back to say, what if this virus mutates? We are vaccinating with a narrow-spectrum vaccine against one piece of the virus. If that piece mutates, it would be able to escape all of our vaccines. And all it needs to do is mutate once, somewhere in the world. And then all of our major vaccines are moot. Why was that not considered?
What would considering it have meant?
For example, the U.S. could have said, “Okay, we’re going to back two vaccines that are against the spike protein only,” and then maybe try to figure out some other vaccines, like multi-protein vaccines, multi-peptide vaccines live attenuated vaccines, killed vaccines — all different sorts of vaccines. And now we very well might find ourselves totally screwed in a few months, because we have no vaccines that will work as well as we need against a mutant that might arise still, or the ones that have already risen.
And we’re doing so little genetic surveillance of the disease here in the States, we don’t even really know what strains are here. We’re flying blind.
We’d much rather just wait and then blame South America and blame the U.K. Meanwhile, we’re probably getting the identical variants here — not just because they’re being brought in by travelers, but because they are probably being built right here in the U.S. through mutation and viral evolution. But now we can blame it on South America or South Africa and the U.K. instead of blaming it on ourselves.
It’s such a horrible impulse.
We have a country that likes to bury its head in the sand. Look at testing in the medical centers in the U.S. How many medical hospitals and clinics actually tested their staff and their physicians regularly? Nobody. I mean, it’s just astounding. But they’d rather bury their head in the sand so that they didn’t even know if transmission was happening in their hospital, because they’d rather not know, because there’s economic cost to that.
The lack of genomic surveillance is just another part of not caring. But rapid testing is another. I’ve been so angry at people like Mike Osterholm saying the only approach is to lock everything down. We have other solutions, we just haven’t used them. We could’ve at least tried, back in May, to get these rapid tests out. We didn’t do it in May. We didn’t do it in August, November, December. We still haven’t done it, but it is one of the only tools that could have actually allowed us to open up safely and gather safely. People talk about COVID fatigue, but then they say, yeah, there’s COVID fatigue, but we need to lock down anyway, because we need to control the virus.
In November I remember seeing articles being written suggesting it wasn’t enough to take a test before seeing your family for Thanksgiving, that you needed to avoid Thanksgiving entirely. I thought that seemed really extreme. Like, okay, sure, these tests aren’t perfect, but they’re not that far, and if you’re telling people they can’t make one exception, armed with a negative test, for a holiday like Thanksgiving, you’re basically telling them they can’t have a meal with anyone but immediate family until May.
People are treating these tests like they don’t work, but, you know what? They do work. But from certain public-health figures you hear this constant refrain, if there is any risk whatsoever, then don’t do it. Somehow these same people are failing to recognize that we have massive risks around us every day, because cases have been completely out of control.
You can’t really take a zero-tolerance approach to risk, even if you want to.
In my opinion, you would actually be safer going in and having a party with people, indoors, if everyone tested right before that party, than you would be going about your regular environment out in the world.
Of course, those risks change a bit as the seasons change, and you said a minute ago that we may already be seeing a shift in seasonality, though we’re just in the middle of winter. When we’ve talked before about the seasonality of the disease, we’ve talked through the conventional list of things that are understood to contribute — temperature and humidity, some effects within the body and immune system of individuals, social dynamics such as indoor socializing and school openings.
One thing that I’ve been mulling over lately is the role of sunlight and vitamin D. I don’t know if you saw, there was a Nature paper a couple of weeks ago looking at the timing of outbreaks across Europe in the fall, which found that there was basically no statistically significant relationship to temperature and humidity, but a significant relationship just to latitude, which is a proxy for sunlight. And when I look at the curves of caseloads and Rt across the country, it’s not that every state is exactly the same, but it does seem that sometime between December 20th and December 30th is the peak in a huge number of these places — right when the days start getting longer again. Is it crazy to be thinking that sunlight effects could be part of the seasonal package? How do you see it?
No, I don’t think it’s crazy at all. I think there’s a lot we don’t fully understand about immunity and the cycles of immunity and how strong our immune systems are during the winter. It’s a huge thing. How many kids get really bad colds and come home all snotty during the summer? The winter — it’s a real thing! But we don’t fully understand why. And vitamin D and sunlight could certainly play a role. Generally scientists and biologists and even physicians oddly throw the most natural explanations under the bus, and say no way. But we are evolved creatures — we evolved on Earth without roofs over our head. It’s insane to think that something like sunlight would not affect us in some way. And we know people get seasonal depressive disorder because of a lack of sunlight, so very clearly it has major impacts on us, and to discount it just because it’s sunlight and not some molecule that …
You can sell.
Yeah, exactly. I’m always astounded at how many physicians just immediately discount all this stuff. We know that vitamin D has a huge interaction with immunity, that’s not even in question. And so I definitely think that could very well be part of it. Is it the primary source of variance or is it just a piece of the puzzle? I would probably say it’s likely a piece of the puzzle.
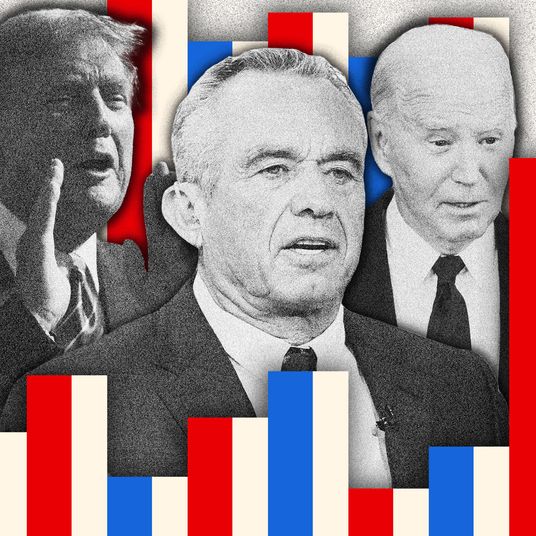
You mentioned the variants earlier, as a sort of wild-card factor. What role do you expect they will play? How scared should we be? Do we know yet?
This is one of the more recent things that I kind of have gotten in arguments with some other scientists about. I said, “If the variants are not as susceptible to immunity acquired by natural infection, then there’s no reason to think that the vaccine would be any different than the natural infection-acquired immunity.” And so many people say, “Well, we haven’t seen the data for that, we need to actually see that vaccine-derived immunity is not performing as well for the variants before we can possibly say that, because it would be too scary to say it.”
But, like, use immunology and biology 101. We created the vaccines to look exactly like the natural virus. We don’t need the data. We don’t actually need it to be able to say, if there are natural strains that are coming about that are evading one version of this virus, then they would also evade the immunity derived by the vaccine. We don’t need the empirical data to start talking about it, because you know, what if it means that policy-makers need to really shift gears and plan for a future in which maybe the vaccines don’t work as well?
Presumably we’d want to be moving really fast then.
We should be setting everyone up as quickly as possible to do that. But the concern about bringing any of that public has been immense. It was like, “Oh wait, you know, that could cause the whole population to be extremely scared and lose faith.” But it’s better to give people the truth now and bring them into the conversation, rather than saying we don’t know enough yet, and then, months later, we say, “Oh, well, actually we did know enough.”
I saw one article suggesting that even those vaccine manufacturers now working on tweaking the vaccines to better address the new variants were saying that the new vaccines wouldn’t be available before 2022, mostly because of regulatory roadblocks. And I thought, well, if we know that the vaccine platform is basically safe, and we have reason to think the first generation of vaccines are less effective against the new strains, and the new strains are spreading quickly, maybe we should be trying to move a little faster even than we did to get the first generation out?
Yeah, exactly. I fully agree. We went truly from zero to a hundred with the current vaccine in less than a year. Why would it be a multiyear timeline to get a new version of the vaccine out? That doesn’t make any sense. But our sense of urgency keeps swinging back and forth. People are kind of picking and choosing where they say things can and should be accelerated versus not.
Why?
I think people have a really hard time not falling back into old ways. In the case of vaccines, there’s such a history of slowness, that when people are then placed in a position to comment on it, their brain just immediately reverts back to thinking that anything really robust and fast is impossible. People allow themselves to see barriers much more than they allow themselves to see solutions.
Yeah. I think in this particular case, one other factor may be that there is a kind of collective desire to have the public regard the pace of vaccine development as exhilarating and amazingly fast — which it was, by any historical standard — but also to not acknowledge that it may even have moved faster. In other words, if we want to celebrate the arrival of the vaccines, and we want the public to celebrate the speed of the development and the testing and the rollout, it almost trains your brain to think, well, that’s got to be the fastest we could do, and it must also therefore be the fastest we could manage a next-generation vaccine, too.
I totally agree. I think that that’s a huge piece of it. It’s just like people breaking the five-minute mile or the four-minute mile and things like that. People think, Oh, you’ll never do faster than that. It’s like, well, actually you can break it by leaps and bounds more. You just have to think differently. So many times we hear people say things like the vaccine trials could never have been sped up any faster. Well, yes, it could. Where there’s a will, there’s a way. You could make a whole new vaccine, based in the same technology, and immediately, tomorrow, we could start phase-three trials of a whole new version. They don’t have to be these amazingly expensive billion-dollar trials. These things can actually be done nimbly and quick and easy.
I mean, in theory, you could even go further and say, if we’re comfortable with the safety and we’re in the middle of the pandemic, and these new strains are a real threat, maybe we could even skip the phase-three trial and just roll it out to the public, then measure efficacy from there — if we’re comfortable with safety.
That’s exactly right. We have treated this all so much like it’s normal. It isn’t normal. We’ve been trying to take the same box that we’re used to working with, and just trying to speed it up instead of just saying, what could be a whole different framework for this? We’re in the middle of an emergency, it’s killing millions of people and ruining economies and societies, should we really just be satisfied with slightly speeding up the status quo?
This is my whole issue with rapid tests, too — rapid tests aren’t about just trying to increase the speed at which we do PCR testing.
Rather than infection, they measure infectiousness, and because they are so cheap, you can test yourself all the time, at home, to guide your own behavior.
It’s totally changing the paradigm of what a test is and saying, we’re in the middle of a pandemic. We don’t have to just build up more and more medical laboratory tests. We need to totally flip it on its head and say, “Look, less expensive, less high-quality tests used much more frequently in a whole different capacity than medical testing is a way to stop an outbreak.” But we’ve had such immense resistance to changing anything. In fact, it’s gone the other way. Instead, people have said, “We’re in the middle of a pandemic, we can’t be changing, we can’t be shifting whole paradigms right now.”
A lot of folks I’ve asked recently about the much better performance of countries in East Asia have pointed out that the region has this sort of dry run with SARS and MERS, and that they learned a lot from that — they saw where some of the vulnerabilities were and invested in repairing them in the intervening decades, but also, because of the earlier experience, understood right of the bat this time what would be required to respond to a pandemic. And that’s obviously true so far as it goes, but I also find myself thinking that we sort of had the equivalent of their SARS experience in March. We could’ve learned from that in the interim, in the way that they did. And we really haven’t.
That’s exactly right. This is the whole idea of building the infrastructure for the future. But policy-makers and scientists and the public has consistently had this expectation that the end is only like a month away, so it’s not worth it to build the new factory to build these tests.
What else has worked like that?
Back in April, I was saying we should be scaling up testing and serological testing because the moment the vaccines come around, everyone’s going to want to know their serological status. Essentially none of it has happened. We have still yet to really build the infrastructure in this country.
And the cost of failing to do that is so clear to me now. We have probably a hundred million or more Americans who already had the disease, which means they have some amount of natural protection. And we’re going to be rolling out a hundred million vaccines. If we could keep those two groups separate, then we’d basically get 200 million with some protection. But we may end up with something much closer to just 100 million people, because we may be giving the vaccine to a lot of people who’ve already had the disease.
I was calling for it! I was trying to get these labs set up back in April and May. I was trying to get investment from the Massachusetts government, from other governors, from philanthropy and investors. And I’ve kind of had to bootstrap like a small version of it — four people doing an amazing job now trying to crank through as many serological specimens as possible every day now. But we should have just built the infrastructure with the expectation and understanding that the moment vaccines come around, they would open up a whole other window.
What do you mean by window?
A better way to vaccinate people efficiently. You vaccinate only people who are seronegative. You give only a single dose to people who are seropositive, not two.
Because there’s evidence that people who’ve been sick benefit from one dose but don’t necessarily need a second. That would double the reach of those doses.
There are so many things we could have done, but serology was always for tomorrow. And even today, people are saying, “Well, we’re never going to get it set up for this pandemic, so we should wait until the pandemic finishes and then we’ll invest in surveillance systems for the next pandemic.” You know what, screw that! For all we know the next pandemic could start tomorrow. We don’t know.
We wouldn’t even have had to wait until the vaccines to see the benefits. I know so many people, I think everybody does, who spent the spring and summer saying things like, “I think I might’ve had it, but I don’t know.” And collectively we’ve sort of chosen to continue living in that kind of fearful uncertainty, rather than be armed with clear knowledge of our status and therefore an understanding of our risk profile going forward. It’s really strange.
It is. It is. It’s this paralysis that results when scientists and physicians and policy-makers say, “Well, we can’t really let people know their status at home, because they’ll go out and party.” No, that’s not what’s going to happen, at least not so much that the tests will actually backfire.
It’s like, you don’t avoid telling people they don’t have lung cancer out of fear they might continue to smoke.
Right. Exactly. It’s insane. It’s totally crazy. And so, you’re absolutely right, we have chosen that the best way forward is to live in a state of uncertainty rather than giving people all the tools and information, even if it isn’t perfect. It turns out that in many cases we’d rather not engage with that knowledge at all than have any sources of error in whatever it is we’re doing.
It’s all just been so sad to me, this unwillingness to look to the future and say, in the midst of all of what’s happening today, “What can we do to set us up for down the road?” To say, “Let’s not act like this is going to be done in a few weeks.” Let’s stop that ridiculous thinking and say, “What do we need to do today to set us up for one year from today, so that one year from today we’re looking back and we’re saying, Thank you, prior self, I’m happy you did that.” But we have had zero of that. Just the development of the vaccine. But even there, we took a very narrow view and didn’t really future-proof it.
Right now is always the best time to do these things, to get ourselves prepared for the future. And, you know what, if we spend a billion dollars and we don’t need it for this pandemic? Great, that’s great news. A billion dollars is nothing for a $16 trillion virus. But you know what, the more likely scenario is that we will end up using it.
What’s else do you have in mind?
I’ve been trying for years to start a global immunological observatory to prevent outbreaks just like this. And for years I’ve been told, “This is too expensive. This is too costly. Why would we ever do this? We’ll deal with it when the disease comes around.” Well, you know, now it’s come around and we didn’t have any global surveillance set up for novel outbreaks. But imagine we had started five years ago to build a weather system for viruses. We could’ve potentially prevented this year from happening.
How would you get all that data?
There’s a few things that are constant across the whole globe. Two of them are, when people get sick they get blood tests, and people donate blood, Blood samples taken in pretty much every single town and city in the world. But the moment that the result the doctors wanted to get is done, they throw away the tubes of blood. Well, what if those tubes weren’t thrown away? What if they were all packaged up and sent to a government facility or franchised immunological observatory labs, and processed with a core set of immunological tools that would give you an understanding of all the pathogens people see. And it can all be de-identified, so it wouldn’t be traced back to individuals. It would turn us all into little weather buoys for infectious disease.
And if we can compile those samples, we could then take all these new technologies where we can take a drop of blood, just literally less than a drop, and I could tell you all of the pathogens that you have ever seen in your life.
How is that different from the technology that Theranos was boasting about?
Well, the thing is, Theranos was actually sort of right. That technology works. They just screwed up by lying about how far along they were. They were saying that they were more advanced than they were, and got caught.
And now we’re about where they were saying they were?
It’s not quite the same. But I can tell you all the stuff that your blood has encoded in antibodies. I can now read it. And if we were to do that on a big population scale and start saying, “Hey, let’s use these technologies like this,” we would be able to start generating the data. That would actually allow us to predict with a whole new level of accuracy when these viruses are transmitting, how they’re transmitting, who are the main culprits, where are they?
*A version of this article appears in the February 15, 2021, issue of New York Magazine. Subscribe Now!