Last year Tony Perry made mice that would have been brown-furred grow up white instead. That Perry, a molecular embryologist at the University of Bath, tweaked their coat colour isn’t new – scientists have been making so-called knock-out mice, in which certain genes are disabled, since the technique was invented in 1989. It is a long and cumbersome procedure that involves combining pieces of DNA in embryonic stem cells and mouse breeding.
But Perry, who published his study in December, didn’t use this method. Instead he used a new genome-editing technology that has been taking the scientific world by storm since it was first developed from the bacterial immune system in 2012, and shown to work in human cells in 2013.
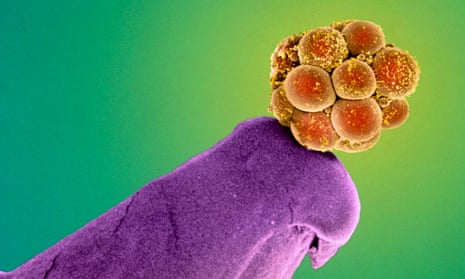
The powerful tool, known as Crispr, allows the precise and easy manipulation of the DNA in the nucleus of any cell. Make the manipulations in sperm, egg or a one-cell embryo, which is just about to start replicating its DNA, and they can become permanently sealed in the so-called germ line, to be inherited by future generations. Using the procedure on the germ line, Perry inactivated a key gene for mouse coat colour.
But Perry’s work added a unique flourish. He did the editing not in a one-cell mouse embryo – which is how most animal germ-line editing by Crispr has been done to date – but earlier, during the process of fertilisation, by injecting the Crispr components and the mouse sperm into the mouse egg at the same time. It is the same technique – intracytoplasmic sperm injection (ICSI) – widely used in IVF. And it worked. “This or analogous approaches may one day enable human genome targeting or editing during very early development,” notes the paper published in the journal Scientific Reports. If human germ-line editing were ever to be used clinically, incorporating Crispr into the ICSI phase of IVF is how it might be.
That prospect tantalises Perry because it raises the possibility of generating offspring that carry either no risk or a reduced risk of some genetic diseases. Perry suggests it might one day be possible to correct a harmful mutation in the BRCA1 gene and stop someone inheriting that predisposition to breast cancer. “You will be able to eradicate it from your descendants,” he says.
Crispr can be thought of as a pair of molecular scissors guided by a satnav. The scissors are a DNA-cutting enzyme; they snip at a precise point in the cell’s DNA specified by researchers using a customised guide molecule, a single short piece of RNA, DNA’s chemical cousin. The DNA-cutting enzyme is known as Cas9, hence the technique is often written Crispr-Cas9.
The genome editing occurs as the cell rushes to naturally repair the break made by the scissors. The cell’s repair often isn’t exact enough for the gene that has been cut to keep working and the gene is effectively knocked out or turned off. More complex to accomplish, though more precise, genes can also be corrected or whole new genes added if a new piece of DNA is included along with the Crispr machinery. It becomes patched in during the cellular repair process.
Germ-line genome editing is highly controversial, even for medical purposes. Since the development of genetic engineering in the 70s there has been a “fairly undisturbed” consensus that human germ-line genetic modification – with the worries it raises about “playing God” and “designer babies” – is off bounds, says Peter Mills, assistant director of the UK Nuffield Council on Bioethics and the council’s lead on genome editing. According to Unesco’s Universal Declaration on the Human Genome and Human Rights, germ-line interventions “could be contrary to human dignity”.
The UK government’s decision this February to allow mitochondrial substitution in the clinic to prevent embryos developing with mitochondrial diseases, a form of germ-line therapy, was premised on the basis that the small amount of DNA mitochondria contain is found outside the cell nucleus. There is no modification to the DNA in the nucleus, the real stuff that makes us who we are.
But there has also never before been a tool shown to be sufficiently effective or reliable enough to seriously consider conducting human genetic engineering. Other precise genome editing tools – Zinc Finger Nuclease (ZFN) and Talen – have been around longer but Crispr is much easier and cheaper to use, accelerating the science and potential applications. “The revolution is in access,” says Dana Carroll, a biochemist at the University of Utah who works on improving the tools. “The technology is developing very rapidly.”
The potential for modifying humans weighs on the minds of some scientists, particularly since the publication last month of a Chinese paper which reported using Crispr to genome-edit human embryos for the first time. (The aim was to correct the gene defect that causes the blood disorder beta-thalassaemia and non-viable embryos, which couldn’t have resulted in live birth, were used.)
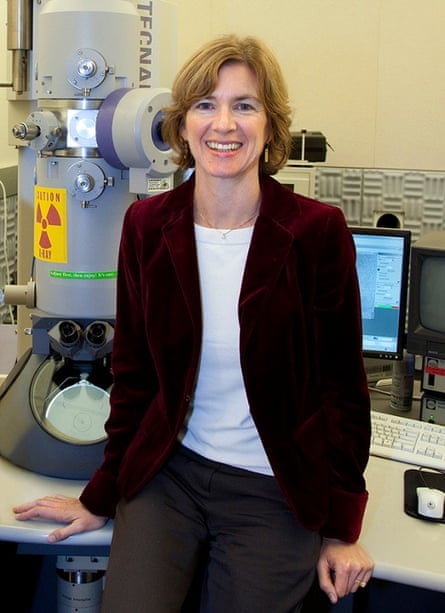
In an opinion piece published in the journal Science in March, a group of US scientists led by the Crispr co-developer Jennifer Doudna from the University of California, Berkeley recommended steps be taken to “strongly discourage” any attempts at germ-line modification therapy that would produce genome-edited humans while the social and ethical implications are considered. They are calling for an international meeting to consider the appropriate way forward for use. “Lets do this now before the technology is applied in ways which people might feel very uncomfortable about,” says Doudna.
A second group writing in the journal Nature went further, suggesting a moratorium on research where human germ cells are edited for fear of where it might lead. The backlash should a modified human be born could, they warn, harm work to develop genome-editing therapy for adults and children where the modifications aren’t passed on. “People might not prise apart the nuances,” says Edward Lanphier, the president and CEO of California-based Sangamo Biosciences, which is pursuing that work.
Indeed, using Crispr in non-reproductive cells – somatic cells – could cure many diseases. Researchers believe it is likely to make it to the clinic sooner. Those modifications can be permanent to the individual’s cells in so far as those cells multiply or remain alive a long time, but they aren’t inherited by future generations. “It has none of the ethical burdens these steps towards germ-line modification would be shouldering,” says Dana Carroll.
The downside is that using Crispr on somatic cells is far more complex: humans have trillions of cells and many different cell types. The genome-tinkering machinery has to be delivered to a sufficient proportion of the specific problem cells to bring about a therapeutic effect.
Thus far, Crispr is too new for any somatic cell editing therapy to have entered clinical trials. But Jennifer Doudna expects them to begin within a few years. “If they go well, I think we could see approved therapeutics within a decade,” she says. In the lab meanwhile, using both human somatic cell cultures and animal models, researchers are experimenting with treating diseases including sickle cell anaemia, severe combined immunodeficiency (SCID), beta-thalassemia, haemophilia, muscular dystrophy and cystic fibrosis. (The approach for these single gene disorders is based on adding a new piece of DNA to correct the faulty gene.)
New companies – Editas Medicine, Crispr Therapeutics and Intellia Therapeutics – have sprung up, licensing Crispr technology to develop somatic cell editing for the clinic. None have yet announced which diseases they are pursuing and a legal battle around who exactly owns the rights to Crispr technology rages. But Intellia has a deal with pharmaceutical giant Novartis to focus on cancer and genetic disorders arising in blood cells.
Somatic cell editing is a sort of upgrade to an earlier technique for curing single gene disorders known as gene therapy. That was first tried in the 90s and hit setbacks. But in 2012 the first gene therapy in Europe – to treat a disease in which a person lacks a protein needed to break down fat molecules – was approved.
Gene therapy introduces a whole new working copy of a gene, which randomly incorporates into the genome to do the job of the faulty one. Genome editing is different in that it precisely targets the existing faulty gene for knock-out or correction. That means the gene’s setting doesn’t change, so doctors neither have to worry that it will incorporate somewhere that causes other genes to be inadvertently turned on, nor that the gene won’t work as normal, for example by not producing the right amount of protein.
“You are keeping everything natural,” says Jennifer Puck, a SCID expert at the University of California, San Francisco, who is exploring the potential of Crispr to treat the disease. Notoriously, in an early trial to treat SCID using gene therapy, the replacement gene incorporated in an unfortunate location and caused leukaemia in five of the 20 patients treated. That problem has been fixed, but the technique can still be tricky to get right.

One challenge shared by Crispr and gene therapy is how to get the gene – or Crispr machinery – inside cells. Methods being adopted from gene therapy to encapsulate and deliver it range from modified viruses to nanoparticles. All are still far from perfect. “People are working hard on delivery and it is problem that will be solved,” says Doudna. “But it is not solved today.”
Delivery is made easier, however, when the cells can be removed for editing. Once outside the body they can be purified, expanded in culture, and checked via genome sequencing to ensure the editing has been successful. That means the early clinical impact of Crispr is likely to be in treating genetic diseases arising in blood cells such as sickle cell anaemia, SCID and beta thalassemia. Doctors are adept at extracting blood and bone marrow (rich in blood stem cells, which give rise to all other blood cells), isolating particular cells for manipulation, and then re-implanting them. Diseases where the cells can’t be removed for treatment will require more work. That includes haemophilia, muscular dystrophy, and cystic fibrosis, which predominantly arise in the liver, muscle and lung cells respectively.
A sense of what Crispr’s future might hold can be seen in the progress of Sangamo Biosciences, which is clinically trialling a somatic cell editing therapy for HIV with efficacy data anticipated by the end of the year. “The goal is to have a functional cure for HIV,” says Edward Lanphier. That would let a patient stop taking antiretroviral drugs for a number of years.
The trial uses the older ZFN technology, for which the company holds the intellectual property rights. The aim, based on replicating a rare naturally occurring mutation that makes some people resistant to HIV infection, is to turn off the CCR5 gene in patients’ T-cells – a type of white blood cell important in the immune system. That gene produces a protein that HIV uses to enter those cells and cause infection.
The ZFNs are put to work outside the body on cells extracted from the patient’s blood. The edited cells are returned in the hope of creating a population of HIV-resistant T-cells that can fight the virus. Just like with Crispr, the custom-designed ZFNs, which come as a pair where a protein structure containing zinc molecules does the guiding, cut the DNA in a precise location – the CCR5 gene – before the cell’s natural but inaccurate repair process kicks in, knocking out the gene. “It really illustrates the power of the approach for treating disease,” says Jennifer Doudna.
Meanwhile, whether editing the human germ line has any clinical future will depend on being able to do it accurately and safely enough, and also whether society finds it acceptable. The conclusion of the Chinese study was that there are still significant technical challenges to be solved before clinical application of Crispr for editing embryos is possible. Problems include “off-target” effects, where the DNA is also snipped at places it shouldn’t be, and “genetic mosaicism”, where the result has a mixture of modified and unmodified cells. Nonetheless, many believe things will improve with more research. It is not safe enough yet, says Robin Lovell-Badge, a researcher who studies germ-cell biology at the Francis Crick Institute, but “it is going to get there fairly soon”.
What specific therapeutic uses might be envisaged? For Lovell-Badge there aren’t many. Pre-implantation genetic diagnosis (PGD) – embryo screening to select those that don’t carry certain disease risks – is already in use for a long list of genetic conditions including the BRCA1 gene, he points out. But he concedes Crispr could have a place when multiple embryos are affected, such as in the case of men who are infertile or sub-fertile because of mutations on the Y chromosome. Any male embryos (produced by IVF) will also have that same mutation.
However, others see wider use. Unlike embryo screening, germ-line editing would not require multiple embryos, which some couples don’t have. It could deal easily with multiple genetic conditions where finding unaffected embryos is a challenge. And it wouldn’t involve discarding any embryos, which some people feel uncomfortable with. “There is an argument for genome engineering in embryos to repair genes that clearly predispose to disease,” says Perry.
Some people may even think it important to use Crispr to make better humans, not just preemptively stamp out disease. There are gene variants which confer extra-strong bones, low Alzheimer’s risk or viral resistance such as to HIV. Beyond that, what about enhancements such as living longer, improved cognition, or altered physical attributes? “I am sure there are broader human characteristics that people would like to be able to modulate,” says Dana Carroll. But he adds that presently those kind of multi-genetic traits would be difficult to edit in because we don’t fully understand their basis, let alone what unintended consequences might result.
The UK has a cautiously progressive regulatory system that would apply to developments in human germ-line editing. Any research on germ cells needs to be licensed by the Human Fertilisation and Embryology Authority (HFEA). Parliamentary approval would be needed for therapeutic use. According to a list of research projects using human embryos currently being carried out in the UK provided by the HFEA, none appear to involve genome editing. But Lovell-Badge says he is aware of “several groups” in Britain interested in using it to “answer some basic research questions”. (Meanwhile the main public funder of research in the US - the NIH - says it won’t fund any use of gene-editing technologies in human embryos.)
It is possible the consensus against modifying humans could change, says Peter Mills, adding that the Nuffield Council is planning a report to consider the ethics of human germ-line editing. There was a new social understanding reached in the UK with the mitochondrial decision; a move from simply selecting human embryos to modifying them. “You can treat [nuclear DNA] as a limit that you don’t cross or a threshold that you very carefully step over,” he says.
If it can be done accurately and safely, human germ-line therapy is a possibility Doudna says she is certainly open to. “People get comfortable with technologies,” she says, citing how over time society has become relaxed about the use of IVF. “I suspect this will be the same.”
Comments (…)
Sign in or create your Guardian account to join the discussion